Migraines: Preventative Care with Acupuncture
/Acupuncture is the technique of piercing the body with a solid needle for therapeutic purposes. Acupuncture was developed in China and the first textbook describing the use of acupuncture is thought to date back to about 200BC. Western interest in acupuncture grew in the 1970’s with President Nixon’s visit to China and has steadily increased since then. The majority of acupuncture treatment in the UK is provided in private practice by professional (lay) acupuncturists who are not from an orthodox medical background. However, acupuncture is provided in almost all NHS pain clinics and by increasing numbers of GPs and physiotherapists.
Types of acupuncture
Two main philosophical approaches are usually recognised. Traditional Chinese medical concepts describe illness and disease as a disturbance of qi (a form of energy or ‘vital force’) within the body. Qi is said to flow along fourteen meridians on the body surface on which the acupuncture points are situated (rather like stations on the lines of the London Underground map). Acupuncture aims to re-establish the correct flow of qi throughout the meridians. Diagnosis may include detailed examination of the pulse and tongue. Needle placement is individualised, so each patient with migraine might receive a different number and distribution of needles. This is often combined with dietary advice and Chinese herbal treatment.
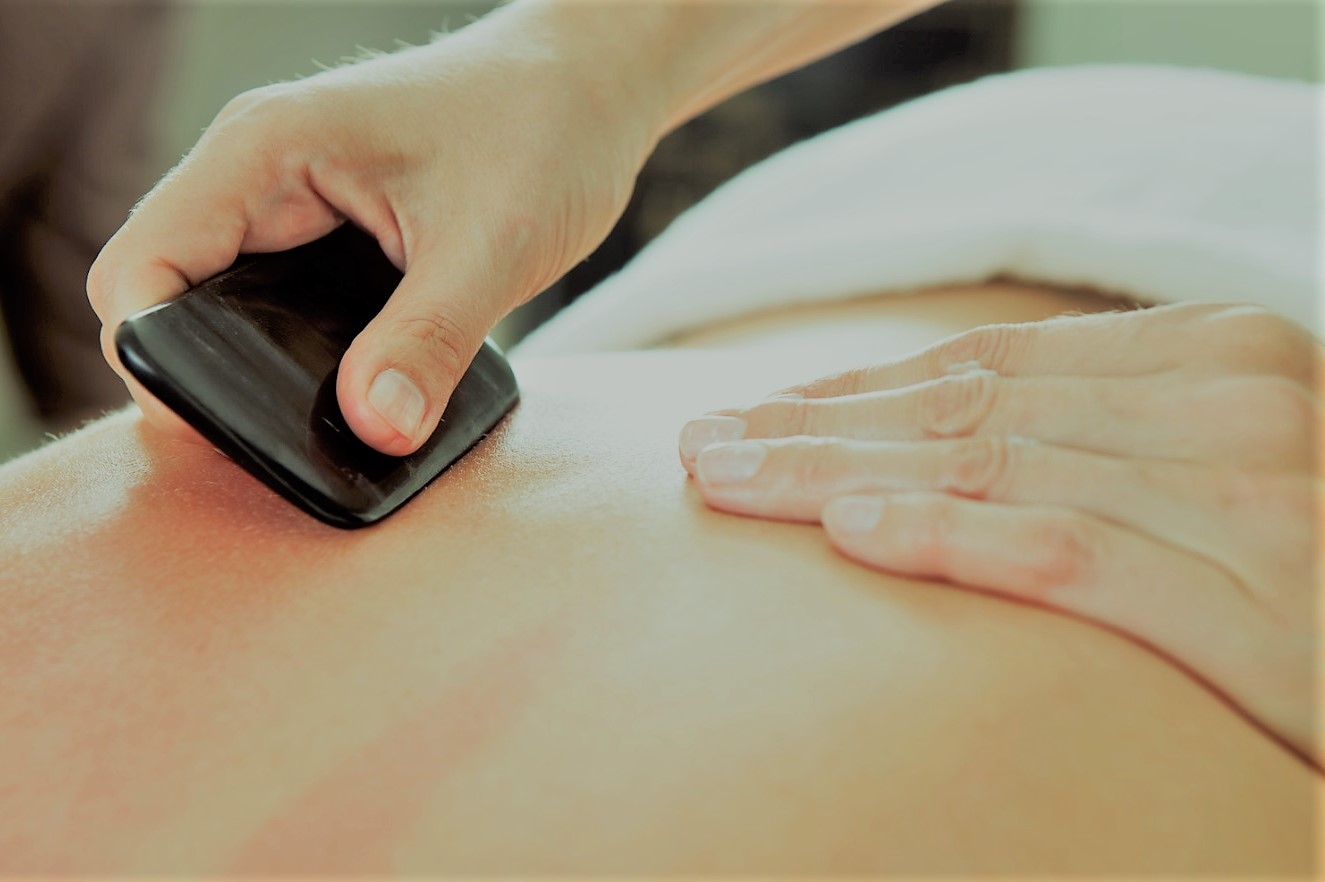
Western medical acupuncture is a modern scientific approach which is based on the biological effects of needling and on clinical and laboratory research. Acupuncture has been found to have effects on the nervous system, including locally where the needles are placed, in the spinal cord and brainstem, where a ‘damping effect’ occurs on pain transmission, and in areas of the brain which regulate the emotional aspects of pain. This may explain beneficial effects from ‘distant’ acupuncture points of traditional practice. Western medical acupuncture uses both local points (for instance on the head and neck) and distant points (such as hands and feet). A related approach is ‘trigger point’ acupuncture, in which tender points in muscles are needled to release muscle spasm contributing to the condition, for example in the neck and scalp.
Evidence for acupuncture
A major problem in acupuncture research is that most clinical trials in headache are ‘randomised, double-blind placebo-controlled trials’, which means that the treatment (typically a drug) is compared with a ‘placebo’ or dummy tablet of identical appearance so that neither the patients nor the researchers know which is which. This is done to minimise treatment expectations affecting the outcome. However, it is much more difficult to devise a ‘placebo’ acupuncture technique with which patients and researchers can be ‘blinded’. One method is called ‘sham’ acupuncture, in which the needles are inserted less deeply into the skin and away from classic acupuncture points. This relies upon the patient not knowing where the true points are and works best in those who have never had acupuncture before. The second method is to use a special needle held in a sheath, which hides it from the patient. The needle can then be made to enter the skin as usual, or to ‘prick’ the skin but not penetrate it (placebo). This has been shown to mimic the sensation of acupuncture effectively. There is much controversy about whether either of these methods are truly inactive like a drug placebo or may have specific effects because they stimulate nerve fibres lying under the skin. The other issue is that practitioners can never be ‘blinded’; they always know which treatment they are giving. For this reason the results of treatment must be assessed by another researcher unaware of which patients got which treatment, or by the patients themselves.
Acupuncture studies in headache have concentrated almost entirely on the prevention of headache rather than acute treatment. A Cochrane systematic review first published in 2001 analysed 16 studies involving 1151 patients and concluded that ‘the existing evidence supports the value of acupuncture for the treatment of idiopathic headaches’, but called for further large-scale studies. Large, randomised controlled clinical trials involving several thousand patients have now been conducted, funded by German health insurance companies. These studies have compared acupuncture with standard treatment (drugs and advice given by physicians) and demonstrate persistent and clinically relevant benefits under real-life conditions and equivalence to specialist drug management. However, no convincing evidence of superiority to ‘sham’ acupuncture has been shown for headache. To skeptics, this suggests that ‘acupuncture doesn’t work’ (i.e. ‘it is no better than placebo’). To supporters of acupuncture, it suggests that while the studies show that it may not matter quite so much how the acupuncture is done, i.e. where the needles are placed or how deeply, acupuncture is much better than no treatment and equivalent to conventional treatment options, with considerably fewer side-effects.
In so-called ‘pragmatic’ studies, the real-world effectiveness of acupuncture has been assessed when given in addition to usual treatment. Patients are randomized to ‘acupuncture’ or ‘no additional treatment (standard GP management) without the use of a placebo. In one such study, patients suffering with chronic headache (80% with migraine) were given 12 sessions of acupuncture over 3 months. This resulted in 34% fewer headache days, 15% less medication, 15% fewer days off work and 25% fewer GP visits after one year. The cost-effectiveness, expressed per ‘quality-adjusted life year’ (QALY), the recommended measure, was £9000 per QALY, well under the threshold of £20-30 000 per QALY) required by the National Institute of Clinical Effectiveness (NICE). These results have been repeated in Europe.
The National Institute for Health and Care Excellence (NICE) include in their headache guideline(2012, updated 2015) that a course of up to 10 sessions of acupuncture may be offered by a healthcare professional if neither topiramate or propranolol are suitable or work well for a particular patient. However, there is no mandate for health professionals to prescribe acupuncture. In practice its availability on the NHS is inconsistent.
Safety of acupuncture
Acupuncture is extremely safe if delivered by adequately trained practitioners. The most frequent side-effects are mild and include: minor bruising or bleeding, usually on needle withdrawal (3%), worsening of existing symptoms (1%) which usually lasts no more than two days and is sometimes associated with a good overall outcome; drowsiness, relaxation, or euphoria (3%) which is often experienced as pleasurable (and if so is not an adverse event!), and pain at the needling site (1%). Severe, extremely rare side-effects include a puncture lung or heart membrane (this is avoided by correct technique); transmission of blood-borne diseases (e.g. hepatitis C), avoided by using single-use, sterile, disposable needles, and skin infection (which is possible with ear acupuncture, particularly if indwelling studs are used).
Acupuncture at the Royal London Homeopathic Hospital
The Royal London Homeopathic Hospital, part of University College Hospital NHS Trust, introduced acupuncture into the NHS in 1977. It is the largest provider of acupuncture services to NHS patients, providing several thousand patient sessions per year. All treatment is provided by conventionally qualified doctors, nurses and physiotherapists who are additionally trained in acupuncture. Both Western and traditional Chinese techniques are used. With increasing scientific evidence for the effectiveness of acupuncture, the RLHH has concentrated on the challenge of providing NHS acupuncture on the scale and frequency required to treat the large number of sufferers with chronic painful conditions including headache and migraine, facial pain, back and neck pain and knee osteoarthritis. It has set up a number of pioneering group treatment services, where patients are treated up to six at a time initially on a weekly or two-weekly basis, followed by monthly maintenance treatment for those who respond. Clinical audit has demonstrated that the results compare with those from clinical trials.
References
Linde K et al. Acupuncture for migraine prophylaxis. Cochrane Database of Systematic Reviews 2009, Issue 1. Art. No.: CD001218.
Diener HC. et al. Efficacy of acupuncture for the prophylaxis of migraine: a multicentre randomised controlled clinical trial. Lancet Neurol. 2006 Apr;5(4):310-6.
Linde K, Streng A, Jurgens S, Hoppe A, Brinkhaus B, Witt C et al. Acupuncture for patients with migraine: a randomized controlled trial. JAMA 2005;293(17):2118-25.
Vickers A. et al. Acupuncture for chronic headache in primary care: large, pragmatic, randomised trial BMJ 2004;328;744-9.
Wonderling D et al. Cost effectiveness analysis of a randomised trial of acupuncture for chronic headache in primary care. BMJ 2004;328;747.
National Institute for Health and Care Excellence. Headaches in over 12s: diagnosis and management (NICE guidelines [CG 150]). 2012 (updated 2015).
this article originally appeared on migrainetrust.org, with contribution by Dr Saul Berkovitz MRCP










![Self-regulation “control [of oneself] by oneself"](https://images.squarespace-cdn.com/content/v1/55563e14e4b01769086817cb/1542845645966-PO2HGKF5JLUBM45UIWQ3/wee-lee-790761-unsplash.jpg)