PTSD: Symptoms, Self-Help and Treatment
/
Overcoming PTSD and Moving On with Your Life
Threatening, deeply hurtful, or very upsetting experiences that leave you feeling helpless and hopeless will trigger a fight, flight, or freeze response, which is your nervous system's reaction to danger. Normally, you recover in a few days or weeks, but when you don't, you may be suffering from PTSD. Painful and disabling as it may be, PTSD is a stress response amenable to change. You can begin doing things to alleviate your PTSD symptoms and take back control of your life.
What is PTSD?
Post-traumatic stress disorder (PTSD) can develop following a event that threatens—or appears to threaten—your safety. Most people associate PTSD with rape and battle-scarred soldiers—and military combat is the most common cause in men—but any event (or series of events) that overwhelms you with feelings of hopelessness and helplessness can trigger PTSD, especially if the event feels unpredictable and uncontrollable.
PTSD can affect people who personally experience a threatening event, those who witness the event, or those who pick up the pieces afterwards, such as emergency workers. PTSD can also result from surgery performed on children so young they don't understand what's happening to them, or an event that leaves you emotionally shattered.
Traumatic events that can cause PTSD include:
- War
- Natural disasters
- Car or plane crashes
- Terrorist attacks
- Sudden death of a loved one
- Rape
- Kidnapping
- Assault
- Sexual or physical abuse
- Childhood neglect
PTSD symptoms: Everyone is different
PTSD develops differently from person to person because everyone's nervous system and tolerance for stress is a little different. While the symptoms of PTSD most commonly develop in the hours or days following the traumatic event, it can sometimes take weeks, months, or even years before they appear. There are three main types of symptoms:
Re-experiencing the traumatic event. This may include upsetting memories, flashbacks, and nightmares, as well as feelings of distress or intense physical reactions when reminded of the event (sweating, pounding heart, nausea, for example).
Avoiding reminders of the trauma. You may try to avoid activities, places or thoughts that remind you of the trauma or be unable to remember important aspects of the event. You may feel detached from others and emotionally numb, or lose interest in activities and life in general, sensing only a limited future for yourself.
Increased anxiety and emotional arousal. These symptoms include trouble sleeping, irritability or outbursts of anger, difficulty concentrating, feeling jumpy and easily startled, and hypervigilance (on constant “red alert”).
Other common symptoms of post-traumatic stress disorder (PTSD)
- Guilt, shame, or self-blame
- Substance abuse
- Feelings of mistrust and betrayal
- Depression and hopelessness
- Suicidal thoughts and feelings
- Physical aches and pains
Symptoms of PTSD in children
In children—especially very young children—the symptoms of PTSD can be different from adults and may include:
- Fear of being separated from parent
- Losing previously-acquired skills (such as toilet training)
- Sleep problems and nightmares
- Somber, compulsive play in which themes or aspects of the trauma are repeated
- New phobias and anxieties that seem unrelated to the trauma (such as a fear of monsters)
- Acting out the trauma through play, stories, or drawings
- Aches and pains with no apparent cause
- Irritability and aggression
PTSD symptoms: How PTSD affects your nervous system
When your sense of safety is shattered by a traumatic event, it’s normal to have bad dreams, feel fearful, and find it difficult to stop thinking about what happened. For most people, these symptoms gradually lift over time. But this normal response to trauma becomes PTSD when the symptoms don’t ease up and your nervous system gets "stuck."
Your nervous system has two automatic or reflexive ways of responding to highly stressful events:
- Mobilization, or fight-or-flight, occurs when social engagement isn’t appropriate and you need to defend yourself or escape the danger of a traumatic event. The heart pounds faster, blood pressure rises, and muscles tighten, increasing your strength and reaction speed. Once the danger has passed, the nervous system calms your body, lowering heart rate and blood pressure, and winding back down to its normal balance.
- Immobilization occurs when you’ve experienced an overwhelming amount of stress in a situation and, while the immediate danger has passed, you find yourself “stuck.” Your nervous system is unable to return to its normal state of balance and you’re unable to move on from the event. This is PTSD.
PTSD self-help tip 1: Get moving
As well as releasing endorphins and making you feel better, by really focusing on your body and how it feels as you move, exercise can help your nervous system become “unstuck”.
- Any rhythmic exercise that engages both your arms and legs—such as walking, running, swimming, or dancing—works well if instead of focusing on your thoughts, you focus on how your body feels.
- Notice the sensation of your feet hitting the ground, for example, or the rhythm of your breathing, or the feeling of the wind on your skin.
- Rock climbing, boxing, weight training, or martial arts can make it easier to focus on your body movements—after all, if you don’t, you could get hurt.
- Aim to exercise for 30 minutes or more each day—or if it’s easier, three 10-minute spurts of exercise.
Spend time in nature
Pursuing outdoor activities like hiking, camping, mountain biking, rock climbing, whitewater rafting, and skiing helps veterans cope with PTSD symptoms and transition back into civilian life. Anyone with PTSD can benefit from the relaxation, seclusion, and peace that come with being out in nature. Seek out local organizations that offer outdoor recreation or teambuilding opportunities.
PTSD self-help tip 2: Self-regulate your nervous system
Learning that you can change your arousal system and calm yourself can directly challenge the sense of helplessness that is a common symptom of PTSD.
- Mindful breathing is a quick way to calm yourself. Simply take 60 breaths, focusing your attention on each out breath.
- Sensory input. Just as specific sights, noises, or smells can instantly transport you back to the traumatic event, so too can sensory input quickly calm you down. The key is to find the sensory input that works for you. Does listening to an uplifting song make you feel calm? Or smelling ground coffee or a certain brand of cologne? Or maybe petting an animal works quickly to make you feel at ease? Everyone responds to sensory input a little differently, so experiment to find what works best for you.
- Reconnect emotionally. Reconnecting to uncomfortable emotions without becoming overwhelmed can make a huge difference in your ability to manage stress, balance your moods, and take back control of your life. See our Emotional Intelligence Toolkit.
PTSD self-help tip 3: Connect with others
Once the fight or flight reflex has been triggered, face-to-face connection with people who make you feel safe and valued is the quickest, most effective way of bringing your nervous system back into balance. The kind and caring support of others can be vital to your recovery. Look for people you can talk to for an uninterrupted period of time, someone who will listen to you without judging, criticizing, or continually being distracted. That person may be your significant other, a family member, a friend, or professional therapist.
If connecting is difficult
No matter how close you are to the person or how helpful they try to be, the symptoms of PTSD that leave your nervous system feeling “stuck” can also make it difficult to connect to others. If you still don’t feel any better after talking, there are ways to help the process along.
- Exercise or move. Before chatting with a friend, either exercise or move around. Jump up and down, swing your arms and legs, or just flail around. Your head will feel clearer and you’ll find it easier to connect.
- Vocal toning. As strange as it sounds, vocal toning is a great way to open up your nervous system to social engagement—even if you can’t sing or consider yourself tone-deaf. Sit up straight and with your lips together and teeth slightly apart, simply make “mmmm” sounds. Change the pitch and volume until you experience a pleasant vibration in your face. Practice for a few minutes and notice if the vibration spreads to your heart and stomach.
- Volunteering your time or reaching out to a friend in need is not only a great way to connect to others but can also help you reclaim your sense of power. Joining a PTSD support group can help you feel less isolated and alone and also provide invaluable information on how to cope with symptoms and work towards recovery.
PTSD self-help tip 4: Take care of yourself
The symptoms of PTSD can be hard on your body so it’s important to take care of yourself and develop some healthy lifestyle habits.
- Take time to relax. Relaxation techniques such as meditation, deep breathing, massage, or yoga can activate the body’s relaxation response and ease symptoms of PTSD.
- Avoid alcohol and drugs. When you’re struggling with difficult emotions and traumatic memories, you may be tempted to self-medicate with alcohol or drugs. But substance use worsens many symptoms of PTSD, interferes with treatment, and can add to problems in your relationships.
- Eat a healthy diet. Start your day right with breakfast, and keep your energy up and your mind clear with balanced, nutritious meals throughout the day. Omega-3s play a vital role in emotional health so incorporate foods such as fatty fish, flaxseed, and walnuts into your diet. Limit processed food, fried food, refined starches, and sugars, which can exacerbate mood swings and energy fluctuations.
- Get enough sleep. Sleep deprivation exacerbates anger, irritability, and moodiness. Aim for somewhere between 7 to 9 hours of sleep each night. Develop a relaxing bedtime ritual (listen to calming music, watch a funny show, or read something light) and make your bedroom as quiet, dark, and soothing as possible.
Helping a loved one with PTSD
When a loved one has PTSD, it takes a heavy toll on your relationship and family life. You may have to take on a bigger share of household tasks, deal with the frustration of a loved one who won’t open up, or even deal with anger or disturbing behavior. The symptoms of PTSD can also result in job loss, substance abuse, and other stressful problems.
- Don’t pressure your loved one into talking. It is often very difficult for people with PTSD to talk about their trauma. For some, it can even make things worse. Never try to force your loved one to open up. Comfort often comes from your companionship and acceptance, rather than from talking.
- Let your loved one take the lead, rather than telling him or her what to do. Take cues from your loved one as to how you can best provide support and companionship—that may involve talking about the traumatic event over and over again, or it may involve simply hanging out together.
- Manage your own stress. The more calm, relaxed, and focused you are, the better you’ll be able to help a loved one with PTSD.
- Try to prepare for PTSD triggers. Common triggers include anniversary dates; people or places associated with the trauma; and certain sights, sounds, or smells. If you are aware of the triggers that may cause an upsetting reaction, you’ll be in a better position to help your loved one calm down.
- Don’t take the symptoms of PTSD personally. If your loved one seems distant, irritable, angry, or closed off, remember that this may not have anything to do with you or your relationship.
- Educate yourself about PTSD. The more you know about the symptoms, effects, and treatment, the better equipped you'll be to help your loved one, understand what he or she is going through, and keep things in perspective.
- Take care of yourself. Letting your family member’s PTSD dominate your life while ignoring your own needs is a surefire recipe for burnout. You need to take care of yourself in order to take care of your loved one.
Professional treatment for PTSD
Treatment for PTSD relieves symptoms by helping you deal with the trauma you’ve experienced. A doctor or therapist will encourage you to recall and process the emotions you felt during the original event in order to reduce the powerful hold the memory has on your life.
You’ll also:
- Explore your thoughts and feelings about the trauma
- Work through feelings of guilt and mistrust
- Learn how to cope with intrusive memories
- Address problems PTSD has caused in your life and relationships
Types of treatment for post-traumatic stress disorder (PTSD)
- Trauma-focused cognitive-behavioral therapy involves gradually "exposing" yourself to feelings and situations that remind you of the trauma, and replacing distorted and irrational thoughts about the trauma with more balanced picture.
- Family therapy can help your loved ones understand what you’re going through and help the family work through relationship problems.
- Medication is sometimes prescribed to people with PTSD to relieve secondary symptoms of depression or anxiety, although they do not treat the causes of PTSD.
- EMDR (Eye Movement Desensitization and Reprocessing) incorporates elements of cognitive-behavioral therapy with eye movements or other forms of rhythmic, left-right stimulation, such as hand taps or sounds. These work by "unfreezing" the brain’s information processing system, which is interrupted in times of extreme stress.
Finding a therapist for PTSD treatment
When looking for a therapist, seek out mental health professionals who specialize in the treatment of trauma and PTSD. You can ask your doctor or other trauma survivors for a referral, call a local mental health clinic, psychiatric hospital, or counseling center, or see the Resources and References section below.
- Choose a PTSD therapist who makes you feel comfortable and safe.
- If a therapist doesn’t feel right, look for someone else. For therapy to work, you need to feel understood.
This article originally appeared on helpguide.org and was written by Melinda Smith, M.A., Lawrence Robinson, and Jeanne Segal, Ph.D.
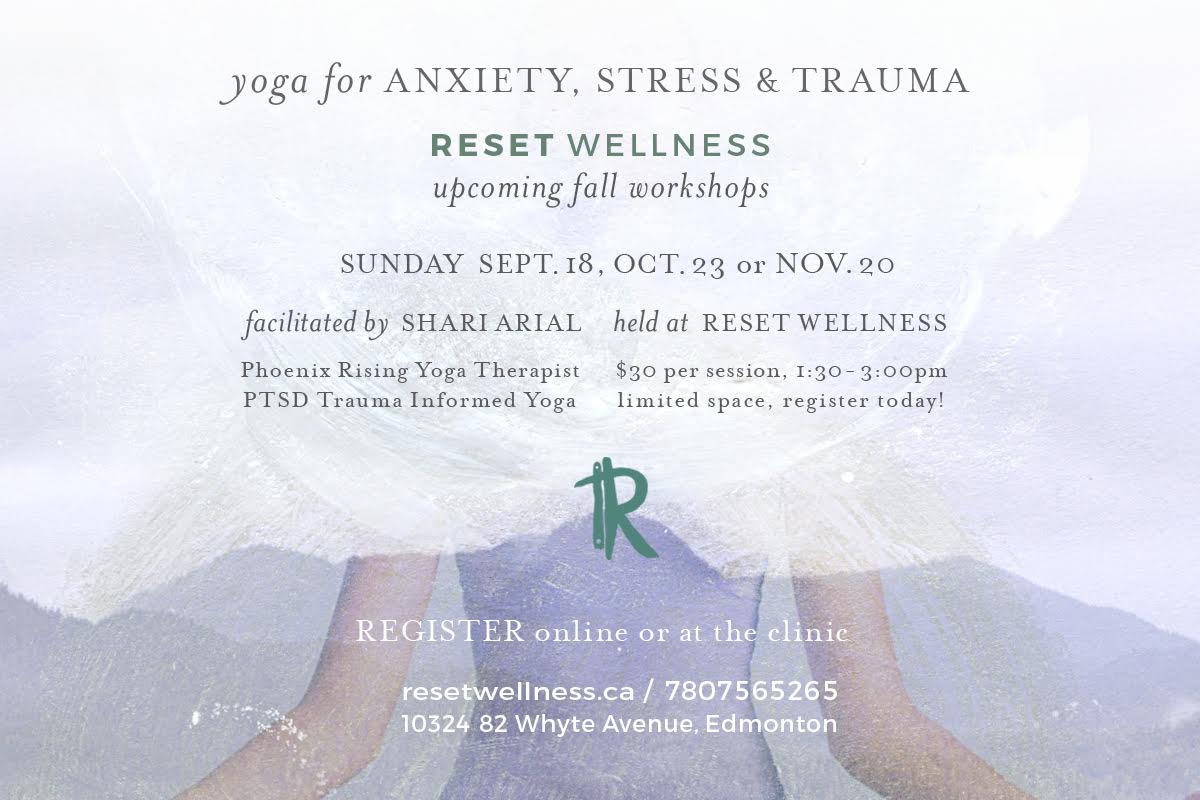
YOGA for Anxiety, Stress & Trauma Workshops offered monthly at Reset Wellness.
For more information see our class listing on our website.











![Self-regulation “control [of oneself] by oneself"](https://images.squarespace-cdn.com/content/v1/55563e14e4b01769086817cb/1542845645966-PO2HGKF5JLUBM45UIWQ3/wee-lee-790761-unsplash.jpg)